The Ten Defining Characteristics of a Well-Formulated Ketogenic Diet

Despite the increasing popularity and the common use of the term ‘keto’ or ‘ketogenic’ to describe carbohydrate restricted diets, in our experience many of the people who use these terms to describe their daily nutrient intakes are not actually on a ‘ketogenic’ diet by objective criteria. More importantly, of those who do achieve nutritional ketosis, many are consuming poorly formulated ketogenic diets that put them at risk for unpleasant side effects and potential adverse events. To be blunt, this can be hard for many otherwise very capable people to do on their own. It involves a complex mix of timed dietary choices, medication management, and behavioral changes that involve more than just deciding to eat fewer carbohydrates. Thus, most people who make an earnest attempt to self-navigate a ‘keto diet’ either fail in their initial efforts due to inadequate results, preventable side effects, or ultimately give up because what worked for them initially did not prepare them for long-term success.To promote a better understanding of what constitutes a well-formulated ketogenic diet, we have identified 10 key characteristics of both the diet and the context of its use. They are:
- Sustains nutritional ketosis
- Maintains or improves lean body mass and performance
- Effective electrolyte, mineral and hydration management
- Fat provides majority of dietary energy in all phases
- Counting calories is not necessary for success
- Totally or predominantly composed of ‘whole foods’
- Short-term very low-calorie diets should be avoided until proven effective in long term studies
- Contraindicated for chronic conditions unless a credible long-term maintenance phase has been demonstrated
- Ongoing expert medical supervision required for medication management of chronic conditions (e.g., type 2 diabetes, hypertension)
- A well-formulated ketogenic diet does not necessarily adhere to traditional dietary guidelines
Admittedly, this list may appear a bit daunting. However, for many people, the short and long-term health benefits of nutritional ketosis (NK) more than justify the efforts needed to achieve and maintain it. The valuable effects of sustained nutritional ketosis include reduced inflammation¹,² and improved insulin sensitivity³,⁴—in addition to a reduction in hunger and cravings⁵,⁶. In combination, these benefits of NK predictably lead to improved metabolic health and major weight loss. However, it is evident that getting an individual’s blood ketone level into the effective therapeutic range of 0.5 to 4.0 mM and then maintaining it there for months and years can be a major challenge. A thorough understanding of the proper composition and management of a well-formulated ketogenic diet (WFKD) is essential in order to achieve and sustain the benefits of nutritional ketosis. In the short-term, appropriate fluid and electrolyte/mineral intakes that match the unique requirements associated with keto-adaptation are necessary for optimum well-being and can markedly reduce or prevent symptoms of the so-called ‘keto-flu’. Over the ensuing months and years, getting and keeping this formulation ‘right’ for the individual is necessary to optimize and sustain metabolic health, disease reversal (e.g., type 2 diabetes, metabolic syndrome, hypertension), and major weight loss. It is also important to keep in mind that for individuals who start out taking medication for a major disease like type 2 diabetes and/or hypertension, a WFKD is a powerful medical therapy which necessitates day-by-day medication management by an expert physician and team to prevent dangerous drug side-effects. We strongly recommend getting medical supervision before making any dietary changes, especially if you are on medications for blood sugar or blood pressure. A physician can help you safely adjust your medications so that they don’t drive your blood sugar or blood pressure too low. Both hypoglycemic (low blood sugar) and hypotensive (low blood pressure) episodes can be very dangerous. To further explore what constitutes a well-formulated ketogenic diet, here are concise summaries of the 10 necessary basic components and how they are utilized to optimize the benefits of nutritional ketosis and to avoid the common pitfalls of this therapeutic metabolic state.
Defining Characteristic #1: A WFKD must result in sustained nutritional ketosis.
- Due to individual variations in carbohydrate tolerance, total daily carb intake can range from nearly 0 to 100 g/d (although tolerance of more than 70 g/d when consuming adequate protein is uncommon). Note: due to wide variations in total energy intakes in the various phases of nutritional ketosis, specifying carbohydrate as a percent of daily intake (aka ‘macros’) is of marginal utility.
- Based upon a combination of clinical experience and known mechanisms through which the ketone beta-hydroxybutyrate (BOHB) functions as both a fuel and regulatory signal, we have defined nutritional ketosis as an average serum BOHB concentration in the range between 0.5 mM and 4.0 mM as measured by validated blood or serum assay methods.
- Despite its reduced carbohydrate content, it needs to be tastefully prepared with adequate variety so as to be palatable and sustainable.
Defining Characteristic #2: A WFKD has to provide adequate macronutrients to preserve lean body mass and function.
- Effective protein intakes can range from 1.2 to 2.0 g/kg-d reference weight, where reference weight is based upon sex-based standard values for height⁷,⁸. See protein recommendations.
- In this protein dose range, the addition of dietary carbohydrate is not necessary to maintain lean body mass⁷,⁹.
- The combination of both carbohydrate and protein intakes at the upper ends of an individual’s tolerance range typically drives ketones down out of the NK range, particularly for those with underlying insulin resistance. For this reason, the best practice of a WFKD typically requires holding protein in moderation and adding just enough dietary carbohydrate to allow dietary variety and provide valuable micro-nutrients and minerals from vegetables, nuts/seeds, and berry fruit.
Defining Characteristic #3: A WFKD contains enough electrolytes and intercellular minerals to maintain optimum circulatory, muscle, and nerve functions.
- Adequate sodium and potassium are provided to support circulatory volume and avoid potassium depletion resulting in impaired muscle anabolism or adrenal stress.
- Accelerated renal sodium excretion associated with nutritional ketosis raises the typical adult daily sodium intake requirement to 4–5 g/d with exceptions for those taking medications for hypertension or congestive heart failure.
- Magnesium depletion signs/symptoms such as muscle cramps, muscle fasciculations, and persistent hypokalemia are common in adults due to poor dietary intake combined with medication and/or alcohol effects on renal excretion.
- Magnesium intake often needs to be increased by food choices or supplementation to normalize neuromuscular and cardiac functions as well as lean body mass preservation independent of dietary protein adequacy.
Defining Characteristic #4: In all phases of a WFKD, the majority of daily energy intake will come from dietary fat.
- Example: -Induction = 80–120 g/d protein, 30–50 g/d carb, 60–100 g/d fat -Maintenance = 80–120 g/d protein, 30–70 g/d carb, 100–200 g/d fat
- In all phases, the majority of fat needs to come from mono-unsaturated and saturated sources from the foods themselves or as added natural fats.
- Adequate omega-6 essential fats are obtained from whole food vegetable and animal/vegetable protein sources. Omega-6 rich vegetable oil sources should be routinely avoided whenever possible.
- As weight loss stabilizes and glycemic control typically improves over the first year of a well-formulated ketogenic diet, it may be possible to add a small amount of additional carbohydrates back into the diet while still maintaining nutritional ketosis. In such transition periods, it will be important to test both blood ketones and blood glucose values periodically to ensure glycemic control is maintained with the addition of carbohydrate.
- Protein remains relatively constant over this time, while fat intake may increase to meet caloric needs.
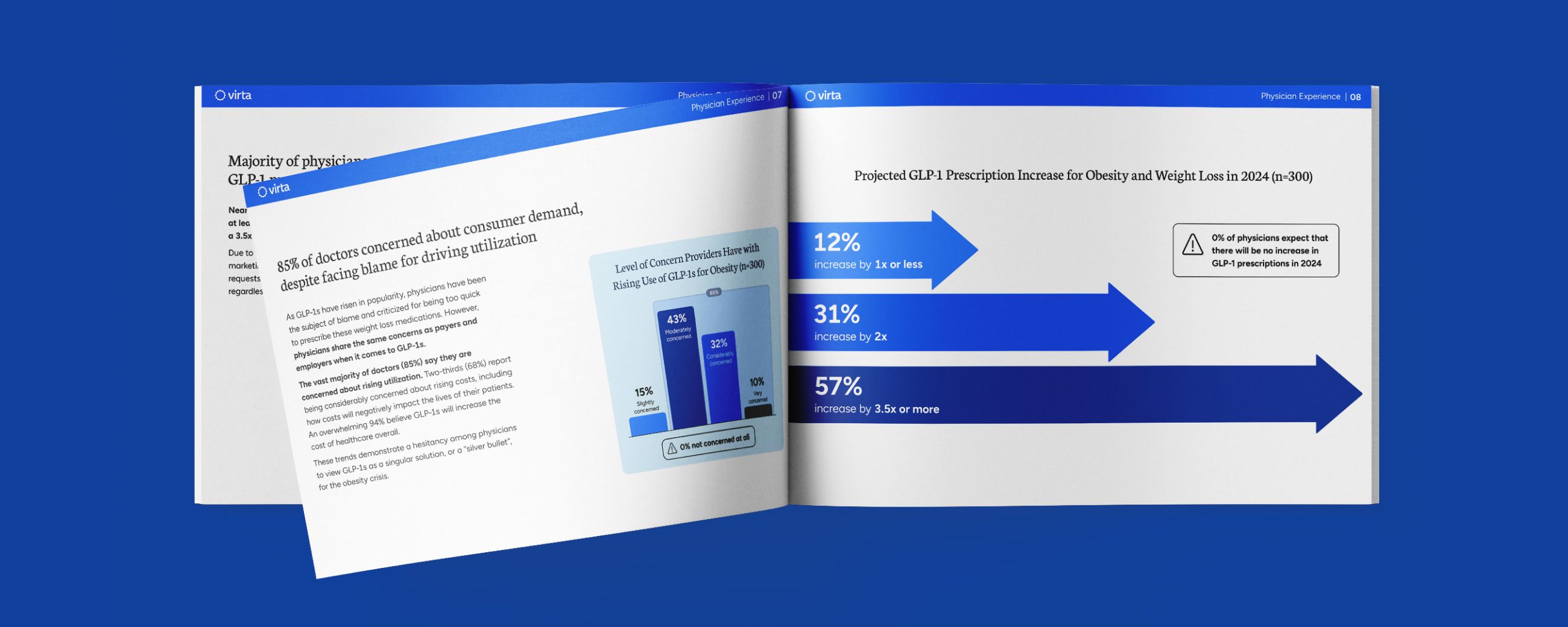
In insulin resistant adults, carbs are initially limited to 30 grams per day, then liberalized slowly while maintaining ketosis. Daily protein prescribed in a range between 1.2 and 2.0g/kg reference weight (approx 15% daily expenditure). Fat is consumed to satiety. This graph illustrates a typical physiological weight loss response to a well-formulated ketogenic diet eaten to satiety rather than when prescribed as a rigid caloric restriction. Note that in this scenario, dietary protein is moderate and unchanged, carbohydrate is held constant or only slightly increased in a narrow range, and one’s spontaneous intake of fat increases to sustain satiety as major weight loss transitions into weight maintenance.
Defining Characteristic #5: Counting or restricting calories is not necessary for lasting success.
- While many “diets” restrict calories in order to get results, a well-formulated ketogenic diet allows the individual to eat fat to satiety and still lose weight and improve metabolic health.
- Calorie counting is not essential; however, individuals must be mindful not to eat past satiety or purposefully consume fats in excess of energy needs in an effort to increase ketone values.
- For many people who have spent a lifetime eating a fat-restricted diet which promotes inflammation and inhibits satiety, experiencing the prompt sense of having eaten enough (i.e., satiety, not fullness) that occurs with nutritional ketosis can be a new experience. Working with a health coach and/or learning how to identify physiological satiety is important for success.
Defining Characteristic #6: A WFKD is preferably composed of all or mostly whole, unprocessed foods.
- Choose fresh unprocessed vegetables, meats, eggs, dairy, berry fruit, and minimally seasoned nuts and seeds when possible
- Fresh frozen choices with no added sugar and minimal processing are also encouraged
- Fermented foods with no added sugar are allowed (e.g., yogurt, sauerkraut, pickles, kimchi).
- Specialty frozen low carbohydrate meals can be used as needed
- Exceptions to whole foods (electrolyte replacement)- Magnesium- Bouillon (sodium)
- Purified protein sources, specialized fats, high potency vitamin formulations, and meal-replacement formulations (e.g., shakes, bars) in most cases should be used sparingly, but can be helpful to supplement special dietary restrictions like vegetarianism.
Defining Characteristic #7: Any ketogenic regimen under 1000 kcal/d (aka very-low calorie diets (VLCD)), whether from real food or a prepared formula meal, does not qualify as a WFKD due to a lack of adequate macronutrients and calories for long-term sustainability.
To our knowledge there are no published studies of sizeable cohorts fed a VLCD for up to 6 months that did not demonstrate substantial weight regain within 12 months.
Defining Characteristic #8: If intended to treat, manage, or reverse a chronic condition, a WFKD needs to have a credible maintenance phase that can be followed for years and decades.
- For people with underlying insulin resistance in particular, a well-formulated ketogenic diet eaten to satiety frequently allows one to achieve a natural transition into a sustainable maintenance pattern of eating.
- A short-term ketogenic diet or VLCD followed by the re-introduction of carbohydrate in amounts that reverse nutritional ketosis is seldom successful at maintaining weight loss or metabolic health long-term.
- Long-term severe voluntary calorie restriction resulting in constant hunger is NOT a credible, sustainable maintenance strategy.
- High volume exercise, particularly in individuals with a history of diabetes or obesity, is rarely an effective weight maintenance strategy in the absence of some degree of ongoing carbohydrate restriction¹⁰.
Defining Characteristic #9: A therapeutic WFKD requires expert supervision and avoidance of unnecessary cycling in and out of nutritional ketosis.
- If intended to improve diabetes or hypertension, inconsistent and intermittent restriction of carbohydrate intake alone or in combination with restriction of total calories in the context of ongoing medication use adds unacceptable risk of medication side-effects.
- While time restricted feeding or intermittent fasting for periods less than 24 hours may be tolerated within the definition of a WFKD, any fasting longer than 24 hours, even if infrequent, is not likely to confer long-term benefits for those with chronic medical conditions¹¹,¹².
Defining Characteristic #10: A well-formulated ketogenic diet does not necessarily adhere to traditional dietary guidelines.
- A well-formulated ketogenic diet has characteristics that cannot be consistent with traditional dietary guidelines. Thus, it is important to realize that most prevailing dietary dogma and nutrition guidelines in developed countries are inconsistent with the characteristics outlined here.
- A “ketogenic diet” that is very energy restricted but contains a substantial carbohydrate content (e.g., 50% or more of energy), moderate protein, and low-fat is not a well-formulated ketogenic diet⁹,¹³.
- Always consult with a trained physician when beginning a well-formulated ketogenic diet, especially if you have any health conditions and/or you are taking any medications.
- To be clear, this list of defining characteristics is inclusive. If all of these ten characteristics are not addressed correctly, it is likely not a well-formulated ketogenic diet.
Nutritional ketosis achieved by consuming a well-formulated ketogenic diet can be a safe and sustainable therapy for a variety of conditions, particularly those driven by underlying insulin resistance or inflammation. To have a lasting effect, however, in most cases the physiological blood ketone levels characteristic of nutritional ketosis need to be maintained, along with adequate intake of electrolytes and minerals. When used to reverse disease states requiring medication withdrawal, constant medical oversight during the early phases of the dietary intervention is needed. While very restricted prepared formula or food-based diets can have dramatic short-term effects on body weight and disease reversal, these benefits have proven to be fleeting when viewed one to two years post intervention. In the end, achieving a lasting effect depends upon teaching the patient to consume a properly formulated diet composed of readily available and economical ‘whole foods’ eaten to satiety. With attention to these 10 defining characteristics, we have demonstrated that a safe and sustainable state of nutritional ketosis is within reach for a majority of motivated adults who choose to try it²,⁴.The information we provide at virtahealth.com and blog.virtahealth.com is not medical advice, nor is it intended to replace a consultation with a medical professional. Please inform your physician of any changes you make to your diet or lifestyle and discuss these changes with them. If you have questions or concerns about any medical conditions you may have, please contact your physician.
This blog is intended for informational purposes only and is not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or any advice relating to your health. View full disclaimer
Are you living with type 2 diabetes, prediabetes, or unwanted weight?

- Forsythe, CE., Phinney, SD., Fernandez, ML., et al. Lipids. 2008; 43:65–77 Comparison of Low Fat and Low Carbohydrate Diets on Circulating Fatty Acid Composition and Markers of Inflammation. Lipids. 2008; 43:65–77
- Bhanpuri , NH., Hallberg, SJ., Williams, PT., et al Cardiovascular disease risk factor responses to a type 2 diabetes care model including nutritional ketosis induced by sustained carbohydrate restriction at 1 year: an open label, non-randomized, controlled study. Cardiovasc Diabetol (2018) 17:56
- Boden, G., Sargrad, K., Homko, C. Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes. Ann Intern Med. 2005; 15;142(6):403-11.
- Hallberg, SJ., McKenzie, AL., Williams, PT., et al. Effectiveness and Safety of a Novel Care Model for the Management of Type 2 Diabetes at 1 Year: An Open-Label, Non-Randomized, Controlled Study. Diabetes Ther. 2018; 9:583–612
- McKenzie, AL., Hallberg, SJ., Creighton, BC., et al. A Novel Intervention Including Individualized Nutritional Recommendations Reduces Hemoglobin A1c Level, Medication Use, and Weight in Type 2 Diabetes. JMIR Diabetes. 2017;2(1):e5
- Gibson, AA., Seimon, RV., Lee, CMY., et al. Do ketogenic diets really suppress appetite? A systematic review and meta-analsis. Obesity Reviews. 2015; 6: 64–76
- Phinney SD, BR Bistrian, RR Wolfe, et al. The human metabolic response to chronic ketosis without caloric restriction: physical and biochemical adaptation. Metabolism. 1983;32(8):757-68
- Davis PG, Phinney SD. Differential effects of two very low calorie diets on aerobic and anaerobic performance. International Journal of Obesity.1990;14(9): 779-87
- Hoffer LJ, Bistrian BR, Young VR,et al. Metabolic effects of very low calorie weight reduction diets. J Clin Invest. 1984;73(3):750-8
- Hall, KD. Diet Versus Exercise in “The Biggest Loser” Weight Loss Competition. Obesity Biology and Integrated Physiology. 2013; 21:957-959
- Corley BT, Carroll RW, Hall RM, et al. Intermittent fasting in type 2 diabetes mellitus and the risk of hypoglycemia: a randomized controlled trial. Diabet Med. 2018;35:588-594
- Conceição J, Dores J, Araújo F, et al. Severe hypoglycaemia among patients with type 2 diabetes requiring emergency hospital admission: The Hypoglycaemia In Portugal Observational Study-Emergency Room (HIPOS-ER). Diabetes Obes Metab. 2018; 20(1):50-59
- DeHaven, J., Sherwin, R., Hendler, R., et al. Nitrogen and sodium balance and sympathetic-nervous-system activity in obese subjects treated with a low-calorie protein or mixed diet. N Engl J Med. 1980; 302(9):477-82