
Survey says: the standard of type 2 diabetes care falls short for both patients and providers

To hear more about how continuous remote care differs from the norm, listen to this recorded interview.
Think back to the last time you were sick and went to the doctor. How long did it take you to decide that your symptoms warranted a doctor’s appointment?
A couple of hours?
A couple of days?
If you have ever been a patient, you are probably familiar with the uncertainty involved in deciding whether and when to seek medical care. And, if you are one of the 60 percent of American adults living with at least one chronic condition, you know how challenging it can be when your symptoms take years, rather than days, to develop.
That is why we decided to give traditional outpatient care a checkup. In partnership with a marketing research intern team from Purdue’s Krannert School of Management, we surveyed 168 patients living with type 2 diabetes and 48 healthcare professionals who provide type 2 diabetes care. And, what we found is clear: the challenges patients and providers face when it comes to managing type 2 diabetes may very well be symptoms of an underlying problem with how we treat it.
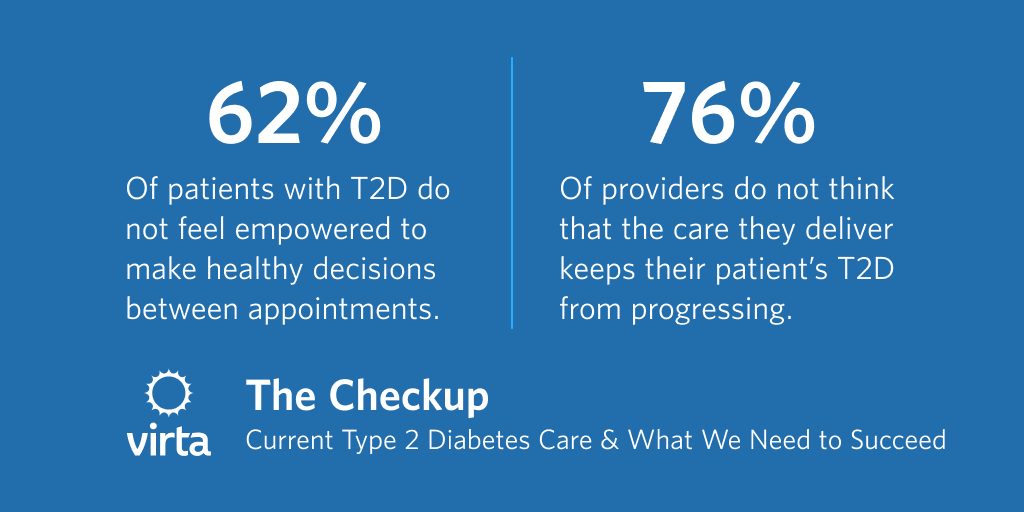
Here’s what we learned: episodic health care every 3 - 6 months does not set patients or providers up for success.

Outside of these visits, patients have to not only follow the prescribed treatment, but also have the wherewithal to know whether or not it is working. And if it is not, it is their responsibility to schedule additional appointments when needed, and to remember details of their day to day symptoms even when the next appointment could be six months down the road.


There’s a tendency to focus on patient shortcomings, but perhaps the issue is that the existing standard of care isn’t setting patients up for success.

Type 2 diabetes is an epidemic whose incidence rate adds 1.5 million new cases every year and amounts to a staggering $327 billion total cost in the United States alone. In the existing care model, providers only have on average 20 minutes to discuss their patient’s progress and develop a treatment plan. So, if our current model is not working, what would it take to shift value in healthcare and affect type 2 diabetes prevalence in the U.S.?
Instead of incremental improvements to outpatient care, we believe the harder but better path forward is continuous remote care. In this system, biomarker data from a patient is automatically uploaded to their electronic medical record (EMR). And from there, artificial intelligence can surface trends to physicians dedicated to this care model, so they could be the ones to reach out to patients the day medical expertise is needed, instead of waiting for the next appointment.
This is no small task, but record-breaking funding into incremental improvements has yet to make a dent on this burgeoning epidemic. From an economic standpoint alone, the burden is untenable. Chronic disease accounts for approximately 75 percent of the nation’s aggregate healthcare spending, and 96 cents per dollar for Medicare and 83 cents per dollar for Medicaid are spent on chronic disease.
To give these individuals and their families a chance to live healthier and more productive lives, we need to address the realities of this disease. Type 2 diabetes is a modern epidemic, and we need to question the norms around how care for it is delivered.
Thank you to our Purdue student team, led by Professor Jinsuh Lee, MS, PhD: Yuefan Jiang, Jia Dai, Tingxuan Kang, Danyang Li, Boxiang Jin, and Nan Ma
This blog is intended for informational purposes only and is not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or any advice relating to your health. View full disclaimer
Are you living with type 2 diabetes, prediabetes, or unwanted weight?






.jpg)

